Cancer researchers from all over the world attended the annual meeting of the American Society of Clinical Oncology, where MSK doctors and scientists presented important research.
Researchers from Memorial Sloan Kettering Cancer Center (MSK) presented several promising studies on treating rare solid tumors at the annual meeting of the American Society of Clinical Oncology (ASCO). The results of clinical trials focused on mesothelioma and three types of soft-tissue tumors illustrate MSK’s depth and breadth of experience in managing all types of cancer, including those so rare that other doctors may see only a few cases in their whole careers. The ASCO meeting was held May 31 to June 4, 2024, in Chicago.
Among the findings presented by MSK investigators:
An Experimental Immunotherapy for Two Rare Sarcomas
Dr. Sandra D’Angelo
Sarcoma oncologist and cellular therapist Sandra D’Angelo, MD, presented interim results from a phase 2 clinical trial that studied an experimental immunotherapy called letetresgene autoleucel (lete-cel) for treating two types of soft tissue sarcoma: myxoid/round cell liposarcoma and synovial sarcoma. The trial found that 40% of patients (18 out of 45) responded to the treatment, meaning that their tumors shrank. All of the patients in the study had aggressive, metastatic disease that had stopped responding to other therapies.
Lete-cel is given as a one-time treatment. Patients must first have chemotherapy to prepare their immune systems to receive it. Results from the trial showed that the average length of time that patients responded to the treatment was more than ten months, and some patients were still doing well after a longer time. Doctors are continuing to follow those patients.
Lete-cel is a kind of immunotherapy called T cell receptor (TCR) therapy. With this treatment, white blood cells called T cells are removed from the patient and engineered to carry an extra tool that allows them to recognize rogue proteins, or markers, that are hiding inside cancer cells. Dr. D’Angelo, an expert in developing immunotherapies for sarcomas, recently published a study of another promising TCR therapy called afamitresgene autoleucel in The Lancet. With lete-cel, the marker that the treatment targets is called NY-ESO-1.
Soft tissue sarcoma is a rare disease that is diagnosed in only about 13,000 people in the United States every year. It develops in the body’s supportive and connective tissues, including fat, muscle, nerves, and blood vessels. Synovial sarcoma and myxoid/round cell liposarcoma each make up between 10 and 20% of soft tissue sarcomas.
The lete-cel trial, which is overseen by Dr. D’Angelo, is being offered at several hospitals around North America and Europe.
This study was funded by GlaxoSmithKline and Adaptimmune.
Giving Chemotherapy and Immunotherapy Before Surgery Is Safe for Treating Mesothelioma
Dr. Michael Offin
Thoracic oncologist Michael Offin, MD, presented results of a study for pleural mesothelioma, a rare cancer of the chest cavity. This investigator-initiated trial, which was conducted entirely at MSK, looked at the benefits of giving a combination of immunotherapy and chemotherapy before patients have surgery to remove the cancer. It showed that this treatment is safe and well tolerated by patients.
The chemotherapy used in the study was a combination of a platinum drug and pemetrexed and the immunotherapy given was the checkpoint inhibitor drug nivolumab (Opdivo®). These drugs are currently given after surgery or in the advanced cancer setting to try to prevent tumor growth.
Giving systemic treatments before surgery, as was done in this study, is called neoadjuvant therapy. The goal of neoadjuvant treatment is to:
- Shrink the tumor and make it easier to remove
- Reduce the number of cancer cells circulating in the blood, to reduce the chances that the cancer will return
As part of the study, the researchers closely examined the cancer tissue after it was removed to determine how the treatments were working. They are now working toward defining pathologic response (figuring out how well the treatment worked by looking at tissues under the microscope) as well as looking for novel markers in the tumor tissue and blood to predict who may benefit most from this strategy.
Mesothelioma is a rare cancer that is diagnosed in about 3,300 people in the United States every year. It can appear in other parts of the body as well, but pleural mesothelioma is the most common type. Many cases of mesothelioma are caused by exposure to asbestos, a building material that was once regularly used for insulation and fire prevention. Others may be caused by inherited cancer-predisposition genes.
The investigators will continue to study the patients to determine whether the neoadjuvant treatments reduced the chances the cancer would come back. They will also study whether these treatments can be offered to more patients.
This investigator-initiated study was funded by Bristol Myers Squibb.
A Promising New Targeted Therapy for Tenosynovial Giant Cell Tumor
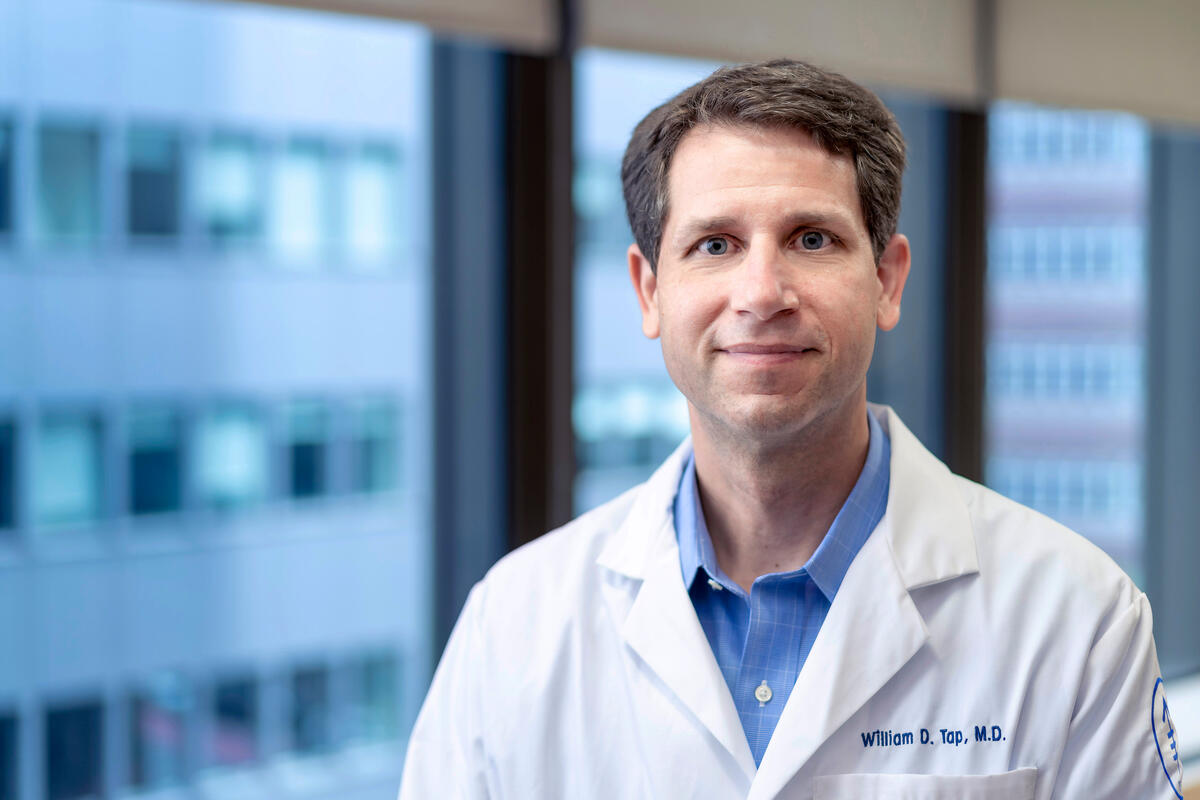
Dr. William Tap
Sarcoma oncologist William Tap, MD, Chief of MSK’s Sarcoma Medical Oncology Service, presented the findings from an international phase 3 clinical trial that studied an experimental targeted therapy called vimseltinib for the treatment of tenosynovial giant cell tumor (TGCT), a rare tumor of the tissue that lines the joints. The investigators found that 67% of patients receiving vimseltinib had measurably reduced tumor volume, compared with none in the placebo group.
Additionally, patients in the trial who received vimseltinib reported improvement in several important measures, including:
- range of motion
- physical function
- joint stiffness
- pain
- overall health
The study was published in The Lancet at the time of Dr. Tap’s presentation, and Dr. Tap was co-corresponding author of the paper.
TGCT, which is also called pigmented villonodular synovitis, is not considered a cancer because it doesn’t spread to other parts of the body. But it can be painful and debilitating, and some people with the disease require multiple surgeries, even amputations. Dr. Tap previously led clinical trials for another drug for TGCT, called pexidartinib (Turalio®). That drug received approval from the Food and Drug Administration in 2019. But because it can cause liver damage in some patients, investigators sought additional options.
This trial found that vimseltinib had far fewer side effects. The most common ones were swelling, rash, headaches, and feeling tired, but none were severe. Importantly, the drug did not appear to cause liver injury in any patients who received it. This is significant because patients need to stay on these medicines long-term to keep their tumors under control. Based on the findings from this study, the researchers say vimseltinib has the potential to become the new standard of care for treating people with TGCT.
This study was funded by Deciphera Pharmaceuticals.